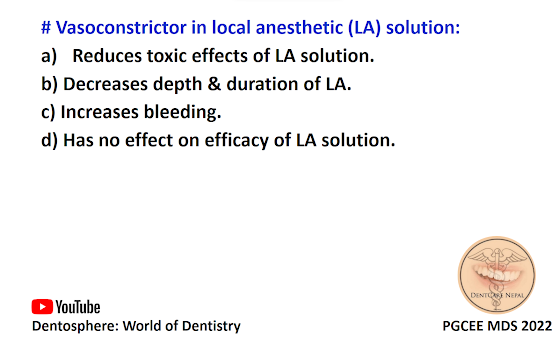
# Vasoconstrictor in local anesthetic (LA) solution:
a) Reduces toxic effects of LA solution.
b) Decreases depth & duration of LA.
c) Increases bleeding.
d) Has no effect on efficacy of LA solution.
The correct answer is A. Reduces toxic effects of LA solution.
Vasoconstrictors are drugs that constrict blood vessels and thereby control tissue perfusion. They are added to local anesthetic solutions to oppose the inherent vasodilatory actions of the local anesthetics. Vasoconstrictors are important additions to a local anesthetic solution for the following
reasons:
1. By constricting blood vessels, vasoconstrictors decrease blood flow (perfusion) to the site of drug administration.
2. Absorption of the local anesthetic into the cardiovascular system is slowed, resulting in lower
anesthetic blood levels.
3. Local anesthetic blood levels are lowered, thereby decreasing the risk of local anesthetic toxicity.
4. More local anesthetic enters into the nerve, where it remains for longer periods, thereby increasing (in some cases significantly, in others minimally) the duration of action of most local anesthetics.
5. Vasoconstrictors decrease bleeding at the site of administration; therefore they are useful when increased bleeding is anticipated (e.g., during a surgical procedure).