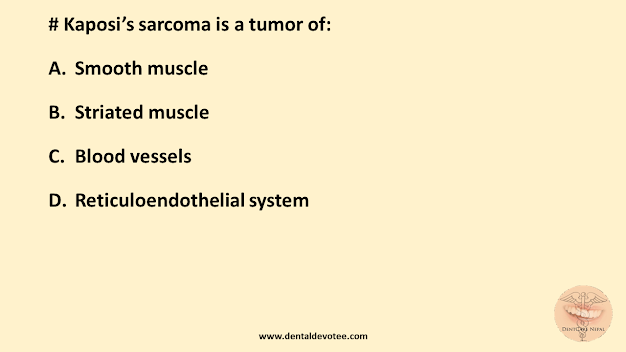
# Kaposi’s sarcoma is a tumor of:
A. Smooth muscle
B. Striated muscle
C. Blood vessels
D. Reticuloendothelial system
The correct answer is C. Blood vessels.
Kaposi’s sarcoma is a low-grade and relatively indolent malignant multifocal tumour of lymphatics or blood vessels caused by infection with human herpesvirus 8 (HHV-8). Its status as a true malignant neoplasm is unclear as it shows a range of behaviours. Most patients are immunosuppressed. Therapeutic immunosuppression with ciclosporin and tacrolimus can be associated with Kaposi’s sarcoma, but by far the main predisposing condition is HIV infection, and almost all oral Kaposi’s sarcoma is in HIV-infected patients. Among HIVinfected patients, Kaposi’s sarcoma affects mainly men who have sex with men. Antiretroviral therapy for HIV has greatly reduced the incidence of Kaposi’s sarcoma, but it remains the most common type of intraoral sarcoma.
Ref: Cawson’s Essentials of Oral Pathology and Oral Medicine, 9th Edition Page no 380