Total Pageviews
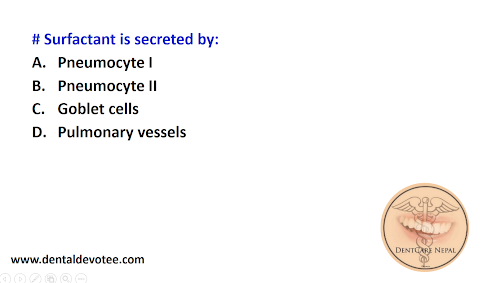
Surfactant is secreted by:
Scleroderma is associated with:
Samaya Dental Care Pvt.Ltd., Kadaghari Kathmandu
Some Sample Intraoral Photograph in Orthodontics
Intraoral Photography in Orthodontics
Determining the Need for Dental Scaling: A Guide for Home Assessment
Maintaining optimal oral hygiene is vital for overall health and well-being. One crucial aspect of oral care is dental scaling, a professional procedure aimed at removing stubborn plaque and tartar buildup from your teeth and gums. While it's always best to consult a dentist for a proper assessment, there are several indicators you can consider to gauge whether your teeth might need scaling. Here's a guide to help you assess the need for dental scaling at home:
Understanding Dental Scaling: Dental scaling, also known as deep cleaning, is a preventive dental procedure designed to remove accumulated plaque and tartar that regular brushing and flossing can't eliminate. Plaque is a sticky film of bacteria that adheres to your teeth and, if not removed, can lead to tooth decay, gum disease, and other oral health issues. Over time, plaque can harden into tartar, which cannot be removed through regular brushing and requires professional intervention.
Signs That Your Teeth Might Need Scaling: While self-assessment can provide some insight, it's essential to remember that only a qualified dentist can provide a definitive diagnosis. However, here are some signs that might suggest the need for dental scaling:
1. Visible Tartar Buildup: Gently examine your teeth in a well-lit area using a mirror. If you notice a yellowish or brownish substance adhering to the tooth surfaces, especially near the gumline, as shown in the picture below, this could be tartar buildup.
2. Bleeding Gums: If your gums bleed while brushing, flossing, or eating, it might be a sign of gum inflammation, commonly known as gingivitis. While bleeding gums can result from various factors, it can be an indication that plaque and tartar are irritating your gums.
3. Persistent Bad Breath: Foul breath that doesn't improve with regular brushing, flossing, and mouthwash might be an indicator of bacteria buildup in hard-to-reach areas of your mouth. These bacteria could be residing in plaque and tartar.
4. Receding Gums: If you notice that your gums are pulling away from your teeth, making your teeth appear longer, it could be a sign of advanced gum disease. Scaling might be necessary to remove tartar below the gumline and prevent further damage.
5. Sensitivity: Increased tooth sensitivity to hot, cold, sweet, or acidic foods and beverages might suggest gum recession due to tartar accumulation. The exposure of sensitive tooth surfaces can lead to discomfort.
6. Visible Cavities: If you can see or feel small holes or pits in your teeth, these could be cavities. Dental scaling might be needed to remove the plaque and tartar surrounding the cavities before they worsen.
Steps to Maintain Good Oral Hygiene:
While self-assessment can be helpful, it's important to consult a dentist for a professional evaluation and treatment recommendations. In the meantime, follow these steps to maintain excellent oral hygiene:
- Brush Regularly: Brush your teeth at least twice a day with a fluoride toothpaste to remove plaque and prevent tartar buildup.
- Floss Daily: Flossing helps remove food particles and plaque from between your teeth and along the gumline.
- Use Mouthwash: An antimicrobial mouthwash can help reduce bacteria in your mouth, promoting fresher breath and healthier gums.
- Maintain a Balanced Diet: Consume a diet rich in fruits, vegetables, lean proteins, and whole grains. Limit sugary and acidic foods and beverages that can contribute to tooth decay.
- Stay Hydrated: Drinking water helps rinse away food particles and bacteria from your mouth, reducing the risk of plaque buildup.
- Regular Dental Checkups: Visit your dentist for regular checkups and cleanings every six months. Professional cleanings can prevent tartar accumulation and catch dental issues early.
Final Thoughts:
While these self-assessment methods can give you some indication of your oral health status, they are not a substitute for professional dental care. If you notice any signs of plaque, tartar buildup, gum inflammation, or other oral health concerns, it's crucial to schedule an appointment with a dentist. Dental scaling, if recommended, can prevent more severe oral health issues and contribute to your overall well-being. Remember, proactive oral care is the key to a healthy smile.
For best result in class III malocclusion correction the orthopedic appliance should be worn at least:
An ANB angle of 2 degrees on the cephalogram usually indicates:
Which condition is associated with mulberry molars in children?
In a hand wrist radiograph, which of the following carpal bones appears first?
Difference of width of four maxillary permanent incisors and primary incisors is about:
Featured Post
Dental MCQs - Multiple Choice Questions in Dentistry
SELECT THE TOPIC YOU WANT TO PRACTICE. # LOK SEWA AAYOG PAST QUESTIONS Medical Entrance Preparation MCQs # Digestive System and Nutriti...

Popular Posts
-
SELECT THE TOPIC YOU WANT TO PRACTICE. # LOK SEWA AAYOG PAST QUESTIONS Medical Entrance Preparation MCQs # Digestive System and Nutriti...
-
NOTE: If you cannot find any books here in the list below, You can search yourself in the Library Genesis Website Database. DISCLAIMER: We ...
-
# Trismus associated with infection of lateral pharyngeal space is related to irritation of the: A. Buccinator B. Masseter ...
-
# All of the following statements about inhaled tooth fragment are true except: A. It usually enters in the right bronchus B. It ...
-
# Parent child relationship has been described as: A. One tailed B. Two tailed C. Three tailed D. Multi tailed The correct answer is A. One...
-
# Growth site of the mandible is in the : A. Body B. Condylar cartilage C. Coronoid process D. Ramus # Maxilla develops by...